EPIDURAL ANALGESIA IN CARDIOTHORACIC SURGERY – DOES IT PREVENT CHRONIC POSTOPERATIVE PAIN?
Interesting Reviews
TEPIDURAL ANALGESIA IN CARDIOTHORACIC SURGERY – DOES IT PREVENT CHRONIC POSTOPERATIVE PAIN?
Eleni Moka
Anaesthesiologist
Heraklion, Crete, Greece
Presented at the Congress ALGOS 2009, Mykonos Island, Greece, June 18 – 21, 2009
for full text in pdf form click here.
for slides – powerpoint presentation click here.
Epidural Analgesia and Cardiac Surgery
The incidence of chronic pain after surgery varies depending on the site of operation. References regarding chronic postoperative pain after cardiac surgery procedures usually focus on the phenomen of poststernotomy neuralgia/pain or dysaesthesia. The frequency of chronic poststernotomy pain after cardiac surgery, according to some authors, fluctuates with percentages climbing up to above 50%, and according to others is found to be around 30%. The incidence of severe incapacitating chronic poststernotomy pain is quite consistently about 3 – 5%, with about one third of these patients reporting that chronic pain disturbs their everyday life and somehow interferes with sleep.
The aetiology is not known, but fractures or incomplete healing of sternum, costal fracture, injury of the brachial plexus and problems related to the use of sternal wire sutures, are mentioned as causes. The use of the internal mammary – thoracic artery (IMA or ITA) has also been suggested to increase the risk, due to intercostal nerves trauma, when dissecting the ITA. Younger patients seem to be at higher risk for long – lasting poststernotomy pain. Additionally, ischeamic coronary pain may sensitize the patient to chronic pain in the same area. In general, chronic pain after cardiac surgery is a problematic area because patients may present re – angina, and differentiating angina pectoris from the post surgery pain may be difficult.
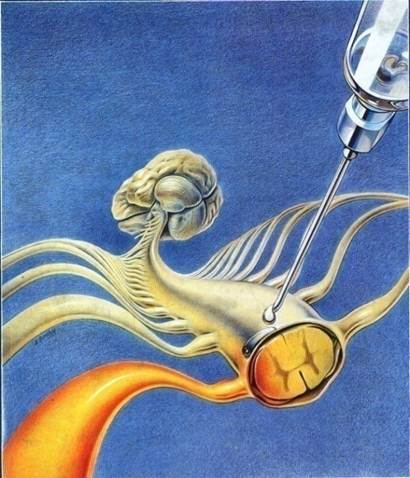
More severe acute pain can signal abnormally severe tissue trauma due to a complication (haematoma, fracture, infection) or nerve entrapment, which then will develop to chronic pain. It is also possible that the endogenous pain control systems are weaker in these patients. The use of high thoracic epidural analgesia (HTEA) has become a frequent supplement to general anaesthesia in cardiac surgery. The potential advantages of HTEA include excellent analgesia, improved pulmonary function, haemodynamic stability, a decrease in stress response to sternotomy and cardiopulmonary bypass (CPB), and reduced risk of depression and post – traumatic stress.
Reduction of painful stimuli in the perioperative period may also reduce central sensitization at the dorsal horns and may attenuate the development of chronic pain. Local anaesthetics, when given epidurally, have the ability to block noxious input to the spinal cord and offer a different mechanism than opiates for modulating the development of chronic pain. However in two papers auditing the role of HTEA in reducing chronic poststernotomy neuralgia, it was not proven that HTEA contributed to a difference in the intensity or frequency of persistent chronic pain following sternotomy, compared with those patients receiving traditional opioid – based analgesia. Local anaesthetics or opioids may not provide total C – afferent blockade during surgery, and inflammation (secondary phase of injury) extends well into the postoperative period and may continue to cause central sensitization, once analgesics are withdrawn. Furthermore, weaknesses in the designing of the two retrospective studies (lack of randomization, relatively small number of patients) could explain why the authors could not find a protective effect of HTEA on chronic poststernotomy pain, neither weak, nor severe pain.
The correlation of the severity of acute pain and the development of chronic pain has previously been suggested. Patients who need more analgesics during the immediate postoperative period are more likely to develop chronic pain after cardiac surgery. Poststernotomy dysaesthesia is a common long term postoperative complication. The association with severity of immediate postoperative pain may indicate a neuropathic element that is usually unrelieved by conventional opioid analgesia. The causative relation still needs to be resolved. Persistent chronic pain following open heart surgery is common and future, prospective, randomized studies addressing the issue are recommended. It is interesting and important to try to elucidate causes and risk factors, because this allows us to look at strategies for prevention, since chronic poststernotomy pain is hard to treat effectively.
Epidural Analgesia and Thoracic Surgery
The development of chronic pain after thoracic surgery is a particularly undesirable, yet common complication. As the study of the pathophysiology of chronic pain with regard to the plasticity of the central nervous system advances, new insights are being gained into not only the potential origins of chronic postthoracotomy pain, but also its potential prevention and treatment options. Thoracotomy, along with limb amputation, is considered to be the procedure that elicits the highest risk of severe chronic postoperative pain. Chronic pain complaints after thoracic surgery (postthoracotomy pain syndrome / PTPS) represent a significant clinical problem in 25 – 60 % of patients. A small subset of these patients experience persistent severe pain, which may be debilitating. Results from thoracic surgical procedures suggest multiple pathogenetic mechanisms that include pre-, intra-, and postoperative factors. The pain may be owing to various causes. Intercostal nerve injury seems to be the most important pathogenetic factor.
Because of the severe pain these patients may experience and the difficulty and expense associated with treatment, prevention may be the best strategy for dealing with this problem. Recent laboratory and clinical studies indicate that minimizing perioperative pain can suppress certain alterations in the nervous system that may prevent the genesis and maintenance of chronically painful conditions. This suggests that strategies for avoiding PTPS may begin with aggressive perioperative anesthetic and analgesic techniques. Thoracic epidural analgesia with local anaesthetics and opioids is regarded as the gold standard treatment for postthoracotomy pain management because it results in early extubation, better ventilator mechanisms and gas exchange, decreased incidence of atelectasis, pneumonia and chronic postoperative pain.
Randomized, double – blind trials on thoracic epidural analgesia (TEA) in relation to PTPS prevention, mainly deal with the concept of timing in relation to a preemptive effect. Preemptive analgesia attempts to reduce post – injury hypersensitivity by early analgesic treatment, prior to surgery, in order to reduce postoperative pain. Only chronic pain following thoracotomy has been found to be preempted by acute pain management and only by continuous thoracic epidural analgesia started before surgery. Recent reviews on effect of preemptive analgesic strategy have presented few trials on the relation to chronic pain, and only five RCTs have evaluated the preemptive effect of analgesia on PTPS. Two of the RCTs including 69 and 58 patients found TEA to reduce PTPS. In contrast, another trial on preemptive use of TEA (112 patients) found no advantage. It seems that the role of TEA on PTPS remains unclarified and questionable. Nevertheless, all of the above studies had insufficient methodology regarding follow up, lack of detailed pain assessment and lack of information on all other potential pathogenetic mechanisms.
In conclusion, the development of PTPS is a particularly undesirable yet common complication. The ongoing research into the development of chronic pain, including that observed after thoracic surgery, portends the development of further advances in options for its control. Further studies regarding the role of TEA are necessary in order to establish multidisciplinary strategies that will provide the foundation for the management of this challenging condition.
Literature
1. Defalque RJ, Bromley JJ. Poststernotomy neuralgia: A new pain syndrome. Anesth Analg, 1989; 69: 81 – 82.
2. Mailis A, Chan J, Basinski A, et al. Chest wall pain after aortocoranary bypass surgery using internal mammary artery graft: A new pain syndrome? Heart Lung, 1989; 18: 553 – 558.
3. Todd DP. Poststernotomy neuralgia: Anew pain syndrome. Anesth Analg, 1989; 69: 692.
4. Eng J, Wells FC. Morbidity following coronary artery revascularization with the internal mammary artery. Int J Cardiol, 1991; 30: 55 – 59.
5. Moore Robert, Follette DM, Berkoff HA. Poststernotomy fractures and pain management in open cardiac surgery. Chest, 1994; 106: 1339 – 1342.
6. Macrae WA. Chronic pain after sternotomy. Acta Anaesthesiol Scand, 2001; 45: 927 – 928.
7. Meyerson J, Thelin S, Gordh T, Karlsten R. The incidence of chronic poststernotomy pain after cardiac surgery – a prospective study. Acta Anaesthesiol Scand, 2001; 45: 940 – 944.
8. Kalso E, Mennander S, Tasmuth T, Nilsson E. Chronic post – sternotomy pain. Acta Anaesthesiol Scand, 2001; 45: 935 – 939.
9. Ho SC, Royse CF, Royse AG, Penberthy A, McRae R. Persistent pain after cardiac surgery: An audit of high thoracic epidural and primary opioid analgesia therapies. Anesth Analg, 2002; 95: 820 – 823.
10. Jensen MK, Andersen C. Can chronic poststernotomy pain after cardiac valve replacement be reduced using thoracic epidural analgesia? Acta Anaesthesiol Scand, 2004; 48: 871 – 874.
11. Alston P, Pechon P. Dysaesthesia associated with sternotomy for heart surgery. Br J Anaesth, 2005; 95: 153 – 158.
12. Taillefer MC, Carrier M, Belisle S, et al. Prevalence, characteristics and predictors of chronic non – angina postoperative pain after a cardiac operation: A cross – sectional study. J Thorac Cardiovasc Surg, 2006; 131: 1274 – 1280.
13. Latinen P, Kokki H, Hynynen M. Pain after cardiac surgery: A prospective cohort study of 1 – year incidence and intensity. Anesthesiology, 2006; 105: 794 – 800.
14. King KM, Parry M, Southern D, Faris P, Tsuyuki RT. Women’s recovery from sternotomy – extension (Wrest – E) study: Examining long term pain and discomfort following sternotomy and their predictors. Heart, 2008; 94: 493 – 497.
15. Wildgaard K, Ravn J, Kehlet H. Chronic post – thoracotomy pain: A critical review of the pathogenetic mechanisms and strategies for prevention. Eur J Cardiothoracic Surg, 2009; in press.
16. Ochroch EA, Gottschalk A, Augostides J, Carson KA, Kent L, Malayaman N, Kaiser LR, Aukburg SJ. Long-term pain and activity during recovery from major thoracotomy using thoracic epidural analgesia. Anesthesiology, 2002; 97: 1234 — 1244.
17. Suzuki M, Haraguti S, Sugimoto K, Kikutani T, Shimada Y, Sakamoto A. Low – dose intravenous ketamine potentiates epidural analgesia after thoracotomy. Anesthesiology 2006; 105: 111 — 119.
18. Hu JS, Lui PW, Wang H, Chan KH, Luk HN, Tsou MY, Lee TY. Thoracic epidural analgesia with morphine does not prevent postthoracotomy pain syndrome: a survey of 159 patients. Acta Anaesthesiol Sin, 2000; 38: 195 — 200.
19. Joshi GP, Bonnet F, Shah R, Wilkinson RC, Camu F, Fischer B, Neugebauer EA, Rawal N, Schug SA, Simanski C, Kehlet H. A systematic review of randomized trials evaluating regional techniques for postthoracotomy analgesia. Anesth Analg, 2008; 107: 1026 — 1040.
20. Moiniche S, Kehlet H, Dahl JB. A qualitative and quantitative systematic review of pre-emptive analgesia for postoperative pain relief: the role of timing of analgesia. Anesthesiology, 2002; 96: 725 — 741.
21. Bong CL, Samuel M, Ng JM, Ip-Yam C. Effects of preemptive epidural analgesia on post-thoracotomy pain. J Cardiothorac Vasc Anesth, 2005; 19: 786 —793.
22. Obata H, Saito S, Fujita N, Fuse Y, Ishizaki K, Goto F. Epidural block with mepivacaine before surgery reduces long-term post-thoracotomy pain. Can J Anaesth, 1999; 46: 1127 — 1132.
23. Hazelrigg SR, Cetindaq IB, Fullerton J. Acute and chronic pain syndromes after thoracic surgery. Surg Clin North Am, 2002; 82: 849 – 865.
24. Koehler RP, Keenan RJ. Management of postthoracotomy pain: acute and chronic. Thorac Surg Clin, 2006; 16: 287 – 297.
25. Gerner P. Postthoracotomy pain management problems. Anesthesiol Clin, 2008; 26: 355 – 367
26. Durá Navarro R, De Andrés Ibáñez J. A review of clinical evidence supporting techniques to prevent chronic postoperative pain syndromes. Rev Esp Anestesiol Reanim, 2004; 51: 205 – 212.






